As the nation’s governors gather this week for their annual meeting in Washington, much of the talk, as usual, will focus on health care. Democratic governors, in particular, are putting forward proposals to make health care more accessible and affordable, specifically for those who still lack coverage. While Washington remains in gridlock, state leaders are moving ahead by using the tools available to them under the existing health care system.
Recent headlines have focused on Democrats’ move to the left. While the political rhetoric in health care revolves around terms such as “single payer,” “Medicare for all,” and “public option,” the reality of the situation is much less dramatic, but nonetheless significant. The substance of the proposed policies in the states consist of achievable and implementable measures that do not require additional federal legislation or creation of new federal programs. Rather, these proposals build on the policies and programs put in place in recent years, including the Affordable Care Act (ACA), and do not disrupt current forms of coverage that almost 92 percent of Americans currently rely on.
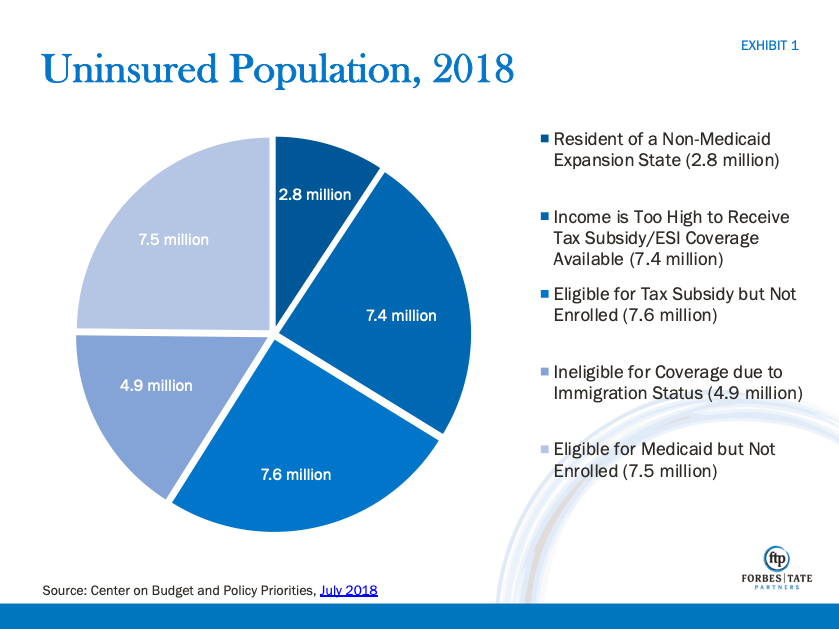
Despite gains over the past several years, there are still over 30 million individuals without health insurance [Exhibit 1]. Already in 2019, state and local leaders are taking actions that directly address segments of the remaining uninsured population. Taken together, they offer a range of solutions that could be implemented locally and cover the vast majority of the remaining uninsured.
- Residents of non-Medicaid expansion states (2.8 million): Significant federal funds are currently available for states to expand their Medicaid programs to cover low and middle income uninsured Americans. However, 14 states have not adopted the program, leaving over 2 million Americans without access to affordable health insurance. Newly elected Democratic governors in Kansas, Wisconsin, and Maine, who ran on the issue, are taking steps to close this coverage gap in their states. In addition, successful ballot initiatives in Nebraska, Utah, and Idaho could close the gap in those states as well.
- Income is too high and employer-sponsored insurance option (7.4 million): Many Americans find health care coverage unaffordable but are not eligible for financial assistance because their incomes are too high to qualify. Others do not receive financial assistance because someone in their household is eligible for insurance through their employer, but because of the so called “family glitch” the cost of that coverage is prohibitive. In California, new governor Gavin Newson is taking steps to address this issue by expanding financial assistance to those who earn more than 400 percent of the federal poverty level (FPL). In Washington, Governor Jay Inslee has proposed a plan to provide additional tax subsidies with the goal of having consumers pay no more than 10 percent of their income in premiums. Finally, New Mexico and Nevada have proposed creating insurance plans that would be available to those who are not eligible for federal financial assistance.
- Eligible for tax subsidy but not currently enrolled (7.6 million): The largest segment of the uninsured population consists of those who are eligible for tax credits to buy health insurance but are not currently purchasing coverage. Many in this population still find coverage unaffordable or live in places without access to health insurance plans that meet their needs. Others simply choose not to buy insurance or are unaware of their options.
- Washington and Colorado have proposed creating new insurance plans to be offered in parts of the states that currently lack more than one insurance plan for consumers to choose from.
- Several states, including New Jersey and Maryland have recently implemented state-backed reinsurance plans to help offset high claims costs incurred by insurance companies. These plans have been shown to reduce premiums and increase affordability for consumers.
- States such as California and New Jersey have proposed or implemented a requirement that everyone have health insurance coverage. This could help bring down costs for everyone by spreading costs and risks among a larger number of people.
- Ineligible due to Immigration status (4.9 million): A sizable portion of the uninsured population consists of those living in the United States without legal status. This situation brings the politically charged issue of immigration into the already sensitive health care debate. Given long standing opposition at the federal level, this population is not eligible for any form of federal assistance for health insurance coverage. Nonetheless, in California, Governor Newsom has proposed making undocumented young people eligible for the state’s Medicaid program. In New York City, Mayor Bill de Blasio has proposed providing access to city funded health care facilities to all residents, regardless of immigration status. While these proposals are likely to be opposed at the federal level, they highlight the willingness of local leaders to use non-federal funds to respond to calls from their base supporters to extend coverage to this population.
- Eligible for Medicaid but not enrolled (7.5 million): A large portion of uninsured Americans are eligible for Medicaid and other health care coverage but are not currently enrolled in those programs. Several states, including most recently New Jersey, have successfully addressed this issue by better integrating programs for low income residents and increasing investment in outreach and enrollment efforts in targeted communities.
With these new policy proposals, state leaders are directly addressing challenges, so all Americans have access to coverage. While at the federal level a stalemate persists on any new action on health care, these leaders are demonstrating significant progress can continue to be made today. And despite a flurry of new terms and charged rhetoric around health care, these proposals highlight the opportunity to make significant, demonstrable progress in access to coverage utilizing existing policies and programs.
